Digestive Health
By Dr Saravana.K


Pancreatic cancer often has a poor prognosis, even when diagnosed early. Pancreatic cancer typically spreads rapidly and is seldom detected in its early stages, which is a major reason why it’s a leading cause of cancer death. Signs and symptoms may not appear until pancreatic cancer is quite advanced and complete surgical removal isn’t possible.
Symptoms
When signs and symptoms do appear, they may include: upper abdominal pain that may radiate to your back; yellowing of your skin and the whites of your eyes (jaundice); loss of appetite; and weight loss.
When to see a doctor
See your doctor if you experience unexplained weight loss, abdominal pain, jaundice, or other signs and symptoms that bother you. Many diseases and conditions other than cancer may cause similar signs and symptoms, so your doctor may check for these conditions as well as for pancreatic cancer.
Factors that may increase your risk of pancreatic cancer include: African-American race; excess body weight; chronic inflammation of the pancreas (pancreatitis); diabetes; family history of genetic syndromes that can increase cancer risk, including a BRCA2 gene mutation, Lynch syndrome and familial atypical mole-malignant melanoma (FAMMM); personal or family history of pancreatic cancer; and smoking.
As pancreatic cancer progresses, it can cause complications such as:
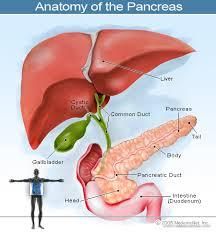
- Jaundice. Pancreatic cancer that blocks the liver’s bile duct can cause jaundice.
- Pain. A growing tumor may press on nerves in your abdomen, causing pain that can become severe.
In severe cases, your doctor may recommend a procedure to inject alcohol into the nerves that control pain in your abdomen (celiac plexus block). This procedure stops the nerves from sending pain signals to your brain.
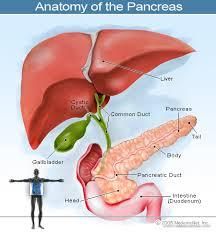
- Bowel obstruction. Pancreatic cancer that grows into or presses on the small intestine (duodenum) can block the flow of digested food from your stomach into your intestines.
- Weight loss.
Diagnosing pancreatic cancer
If your doctor suspects pancreatic cancer, you may have one or more of the following tests to diagnose the cancer:
- Imaging tests include ultrasound, (CT) scan and (MRI).
- Using a scope to create ultrasound pictures of your pancreas. An endoscopic ultrasound (EUS) uses an ultrasound device to make images of your pancreas from inside your abdomen. It is passed through a thin, flexible tube down your esophagus and into your stomach in order to obtain the images. Your doctor may also collect a sample of cells (biopsy) during EUS.
- Treatment for pancreatic cancer depends on the stage and location of the cancer as well as on your age, overall health and personal preferences.
Surgery
Surgery may be an option if your pancreatic cancer is confined to the pancreas.
Radiation therapy and Chemotherapy
Radiation therapy uses high-energy beams to destroy cancer cells. You may receive radiation treatments before or after cancer surgery, often in combination with chemotherapy. Chemotherapy can be injected into a vein or taken orally.
Targeted Therapy
Targeted therapy uses drugs that attack specific abnormalities within cancer cells. The targeted drug blocks chemicals that signal cancer cells to grow and divide.
When pancreatic cancer is advanced and treatments aren’t likely to offer a benefit, your doctor will help to relieve symptoms and make you as comfortable as possible.


