

By Dato’ Dr Amar-Singh HSS & Datin Dr Lim Swee Im
We all know we are in this pandemic for the long haul and may need to maintain prevention measures for the next 2 to 3 years. This means we need sustainable measures that all of us can adhere to and keep for another 2 to 3 years. No one can predict what is going to happen in the next 12 months. Will a viable vaccine emerge? Will the virus change or mutate further? One thing is sure: we will get a second wave and a third wave and a fourth wave. Our aim must be to keep these outbreaks to the bare minimum.
The reasons we are in a better place than some other countries is due to the movement control order (MCO), the hard work and sacrifice by staff of the Ministry of Health (MOH) and public cooperation. There is also some good data emerging that suggests that the COVID-19 mutation spreading in our region is a milder variant with a lower mortality. But this does not mean that other mutations with greater severity will not reach our shores.
However with our low numbers, we see many people who have become relaxed and let down their guard. In addition, fatigue has set in for much of our society and we have become weary in constantly maintaining our vigilance against this virus. We must realise that community spread of COVID-19 is still ongoing; much of it asymptomatic and we can have a flare-up at any moment (as now seen in Kuching).
We want to highlight some important issues that need our consideration, thinking and dialogue as a society. We have summarised them below in the different relevant areas.
How can we Best Monitor our Pandemic when our Numbers are Low?
There are three issues that we should look at, three aspects of data, to monitor the pandemic locally.
The first is to look out for all unlinked cases. These are individuals who test positive but are not linked to any cluster. For example a person coming for an operation who tested positive (a number of these). Or a prisoner about to be transferred is tested positive. All unlinked cases indicate a much larger unrecognised community spread of COVID-19. Their numbers may be small but their implications are huge.
The second is look for infections that are occurring in locations where there is potential for explosive spread, or where fatalities may be high. It is of concern that two prisoners, in two separate prisons (Sabah and Kelantan), were positive. We urgently need the follow-up testing data for both locations to see how many individuals within these cramped, crowded locations are positive.
The third is to monitor the types of COVID-19 mutations that are circulating in Malaysia. In light of growing evidence that severity and fatalities are influenced by mutation type, we need to be updated as to which mutations are circulating and whether new mutations have entered the country.
How Ready are our Testing Capabilities for a Second and Subsequent Waves?
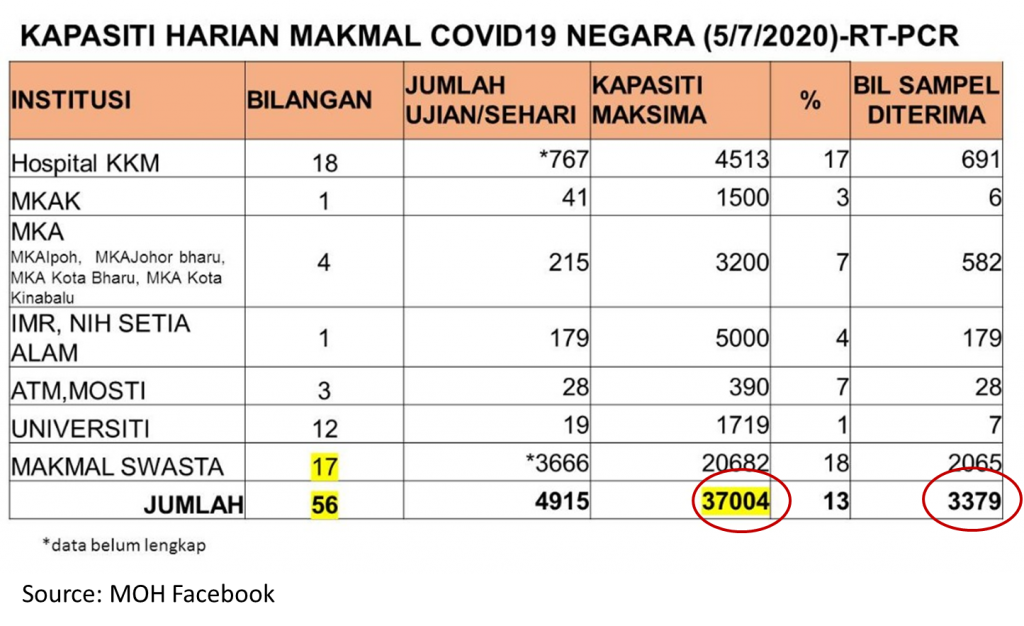
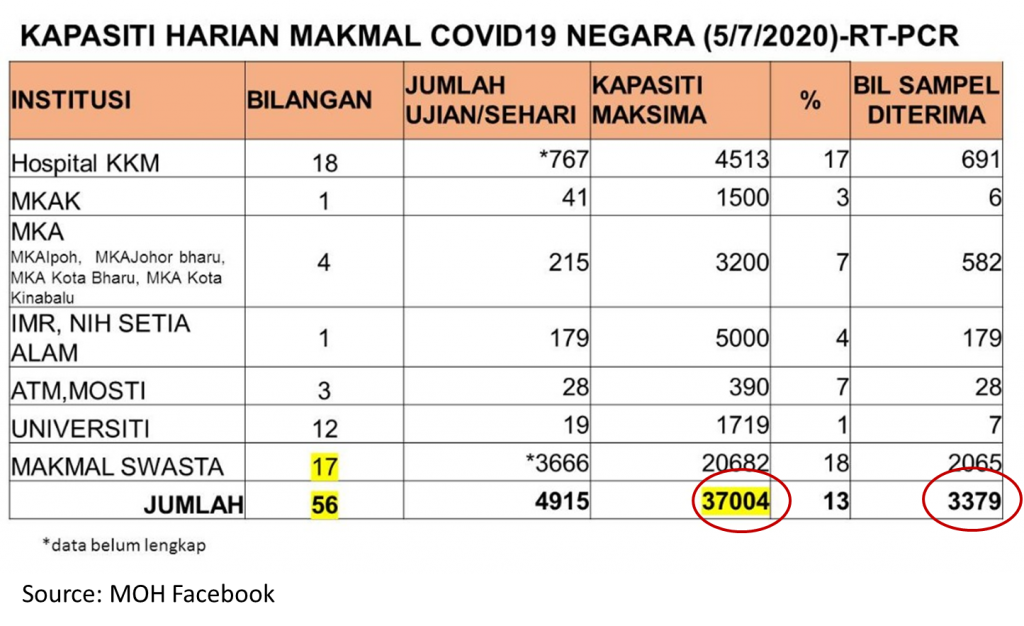
Initially we took some time to ramp up our testing, as we were very slow in receiving results (turn-around time) and slow in expanding to critical areas. We have now improved but appear to have stagnated in total testing capacity. We have been informed, for some time, that we have the ability to do 37,000 PCR tests a day (hopefully with a < 24 hours turn-around time). But is this sufficient if we experience a large surge in cases? A number of countries in our region have significantly increased testing capacity so that they can do large numbers of tests daily. We need to keep growing our testing capacity and exceed 100,000 tests a day to be able to deal with impending subsequent waves, should they come in greater numbers.
Even more worrying is the drop in testing daily numbers. From accessible data, we currently use less than 20% of available tests (see attached graphic). We are not using our tests fully when numbers are apparently low. Now is the time to use all our tests to explore widely and minimise community spread. We should test all frontliners, not just those in hospitals, but police and service individuals (supermarkets, food industry, etc). We should also do exploratory testing, especially in our migrant population (only 65,000 tested as of 15th July 2020). Aggressive testing may have small positivity rates but the returns in stopping community spread may be large, as seen in New Zealand and Taiwan.
How Good are our Safe Physical Distancing Measures?
During the initial MCO, we were ‘forced’ to comply. With relaxation of the order we find many becoming complacent or using masks as a proxy. Masks are very useful but being vigilant with safe physical distancing measures is equally vital. At times we appear to be giving mixed messages. We allow 100% occupancy of air-conditioned aeroplanes, trains and buses but do not permit children in open air playgrounds. We see ministerial and government agencies meeting in closed air-conditioned rooms, often closer than 1 meter but families going out to have a meal together may be fined RM 1,000 each for not sitting apart. We have allowed the resumption of larger religious gatherings and have yet to address the super spreading locations where people are in close proximity like prisons and migrant detention camps. All this suggests we have much to improve regarding safe physical distancing measures.
Optimising Masks in COVID-19 Prevention
The introduction of routine use of masks outside the home is a good and welcome measure in view of asymptomatic spread. It is an important tool in the prevention of COVID-19, especially as safe physical distancing is very difficult in mass transport, smaller offices and in public spaces. It is sad that we have not introduced routine mask use in all our schools, in view of the data from South Korea and Israel that show schools as important parts of the resurgence of COVID-19 in those countries. Face shields used together with masks are also helpful for higher risk individuals or those with greater exposure like frontliners.
There are, however, many issues that must be addressed with a mandatory face mask implementation. Most of us will still remember vividly the old, poor, Chinese uncle who was arrested when he went out to find food during the MCO. We are concerned that the poor will not have the resources to enable them to have face masks. And hence they may be victimized by this measure. There is no way for the poor (B40) to comply with this ruling without a government mandated free programme. Singapore has an excellent system which has dispensed 6 cloth masks to every citizen. However locally some of us have yet to receive the four masks promised to all households nationwide in April 2020.
There will also be a need for a system to exempt some individuals from wearing face masks. Having looked after children for much of my medical life as a paediatrician, I recognise that children with cardiac and respiratory diseases and those who are significantly disabled have difficulty wearing a mask; at times it may even be harmful. This would also apply to some adults. Children under 2 years should also not wear masks. Hence we need an exemption system that is put in place urgently before the mandatory ruling comes into effect.
In addition there are rumours currently circulating about the requirement to only wear 3-ply surgical face masks. We need to have clarity on this issue. It may be dangerous to impose only 3-ply masks as many cannot afford them and will resort to reusing and recycling them, which is hazardous. Already we see 3-ply surgical masks used for the whole day or ironed/sunned and reused. There is also the issue of fake 3-ply surgical masks for sale especially online sales portals.
There are many false graphics circulating on the efficiency of different mask types. We need to retain the N95 masks for medical personnel. 3-ply surgical masks are more effective than cloth masks but cloth masks are useful and there is a growing body of data showing their value. See these reports, studies and summary of the evidence: one, two, three, four, five. In case anyone thinks we cannot deliver free cloth masks to every Malaysian, especially the poor, have a look at the achievement in Singapore and the Czech Republic. Remember that in March 2020 the people of the Czech Republic made hundreds of thousands of cloth face masks for all their citizens and distributed them within 5 days.
Mask Etiquette and our Leaders
The media is full of poor mask etiquette by our leaders. Both the government and opposition members of parliament (MPs) are united in their failure to use masks or their failure to use masks correctly. It is dangerous to wear your mask around your chin and then pull it up to your face as you may infect yourself; however many MPs are doing this. Leaving your nose exposed defeats the function of masks, yet some MPs do this. If you want the people to wear masks please ask our leaders to first lead by example.
We must apply the same set of rules to our leaders as we do to the people. If the people are fined for breaking prevention measures, then the leaders must also be fined. In fact we expect a much higher standard from our leaders. They must show by example so that the people will follow. Blaming the public alone for lack of cooperation is not acceptable. Both the leaders as well as the public must share the responsibility for lapses in prevention measures. We need to encourage each other as we try to deal with the chronic fatigue and depression that comes with this pandemic.
Thank you.


